TOP 10 TAKE HOME MESSAGES
This Chest Pain Guideline was developed for the evaluation of acute or stable chest pain in outpatient and emergency department settings, emphasizing the diagnosis of chest pain with an ischemic etiology.
The following are key guideline perspectives:
-
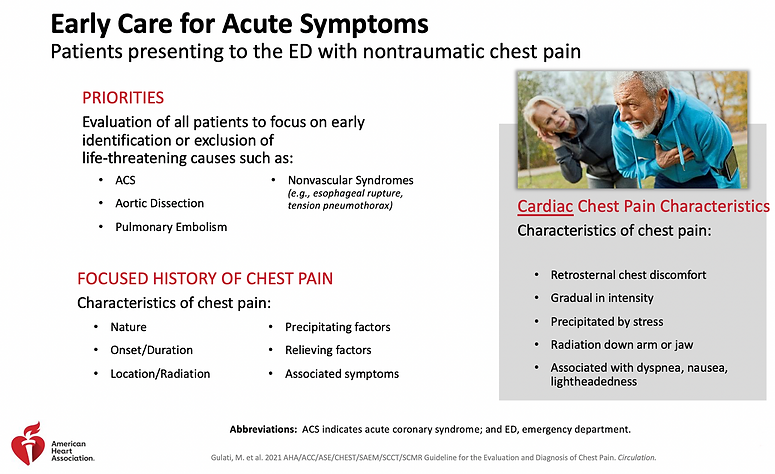
Acute chest pain refers to symptoms of new onset or change from previous in pattern, intensity, or duration; stable chest pain refers to symptoms that are chronic and associated with consistent precipitants. Although the term ‘chest pain’ is used in clinical practice, patients often report pressure, tightness, squeezing, heaviness, or burning in locations in addition to the chest, including the shoulder, arm, neck, upper abdomen, or jaw. Chest pain should be described as cardiac, possibly cardiac, or non-cardiac rather than as typical or atypical.
-
Chest pain is the most common symptom among both men and women diagnosed with acute coronary syndrome (ACS). However, women more commonly have accompanying symptoms including nausea, palpitations, and shortness of breath.
-
Efforts should be made to expedite the evaluation of patients with acute chest pain, including patient education to call 9-1-1 for emergency medical services transportation to the nearest emergency department.
-
Electrocardiography (ECG) is important in the evaluation of both acute and stable chest pain to assess for evidence of ACS.
-
Owing to high sensitivity and specificity for myocardial tissue, serial assessment of cardiac troponin (cTn) I or T is the preferred biomarker for the assessment of myocardial injury among patients with acute chest pain; high-sensitivity cTn is preferred because it allows rapid detection of myocardial injury and has increased diagnostic accuracy.
-
Among patients with acute or with stable chest pain, the use of diagnostic testing should be based on a structured assessment of cardiac risk and targeted to patients most likely to benefit. Clinical decision pathways (CDPs) should be used routinely in the emergency department and in outpatient settings.
-
Clinically stable patients evaluated for chest pain should be included in clinical decision making, weighing information about costs, risks of adverse events, radiation exposure, and alternative options.
-
CDPs for patients with acute chest pain:
-
Among patients with acute chest pain and low cardiovascular risk (30-day risk of death or major adverse cardiac events [MACE] <1%), no additional urgent cardiac testing may be needed.
-
Among patients with acute chest pain at intermediate risk (patients without high-risk features and not classified as low risk) and no known coronary artery disease (CAD), additional testing can include functional testing (exercise ECG, stress echocardiography, stress nuclear myocardial perfusion imaging [MPI], or stress cardiac magnetic resonance [CMR] imaging) or anatomic testing (coronary computed tomography angiography [CCTA]).
-
Among patients with known CAD and acute chest pain at intermediate risk, additional testing can include functional testing or CCTA in the setting of nonobstructive CAD; functional testing in the setting of known obstructive CAD; or invasive coronary angiography (ICA) in the setting of known left main disease, proximal vessel CAD, or multivessel CAD.
-
Patients with acute chest pain and high risk (new ischemic changes on ECG, cTn-confirmed myocardial injury, new left ventricular systolic dysfunction, new moderate-severe ischemia on functional testing, hemodynamic instability, or a high-risk CDP score) should undergo ICA.
Chest Pain Evaluation Guideline (AHA Slides)